Case 4
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 36 year old male who is plumber by occupation came to the OPD complaining about
- Yellowish discoloration of his eyes since 1 month
- Reddish discoloration of urine since 1 month
HISTORY OF PRESENT ILLNESS:
Normal routine of the patient:
He used to get up at 6.30/7 in the morning, used to have tea and passed the time until afternoon talking to his friends then used to have lunch at 1 PM which is rice.He used to return home by 6 in the evening then he used to freshen up and drink alcohol (150-200ml per day) and used to have dinner at 9 PM and sleep after that.
The Patient was apparently asymptomatic 1 month back then he observed yellowish discoloration of his eyes along with reddish discoloration of urine.
He then visited a local hospital for which he was given few tablets. Since the patient didn't find a change, he started taking herbal medication.
He used to have intermittent low grade fever that lasted for approximately one/two hours for which he used to take a PCM tablet.
Since the symptoms didn't subside, he came to the OPD with the same complaints
History of past illness :
The patient is not a known case of diabetes, epilepsy, tuberculosis, asthma, hypertension
Personal history :
- The patient has no loss of appetite
- He takes mixed diet
- No sleep disturbances
- He consumes 150-200 ml of alcohol daily, was a cigarette smoker 5 years back where he used to take 2/3 cigarettes per day.
Family history :
- There are no similar complaints in the family members
Treatment history :
- He is not a known case of drug allergy.
General examination :
- Patient is conscious, coherent, cooperative at the time of joining
- No Pallor
- Icterus present
- No cyanosis
- No clubbing of fingers and toes
- No lymphadenopathy
- No pedal edema
The patient complains of black stools since he started taking medications
Vitals : temperature - 98.4 F
Pulse rate - 84 bpm
Respiratory rate - 18 cycles per minute
BP - 110/80 mm Hg
Systemic examination :
CVS
Inspection - chest wall is bilaterally symmetrical
- No precordial bulge
- No visible pulsations, engorged veins, scars, sinuses
Palpation - JVP is normal
Auscultation - S1 and S2 heard
RESPIRATORY SYSTEM
- Position of trachea is central
- Bilateral air entry is normal
- Normal vesicular breath sounds heard
- No added sounds
PER ABDOMEN
- abdomen is not tender
- bowel and bladder sounds heard
- no palpable mass
- patient has mild amount of fluid
CNS
- Patient is conscious
- Speech is present
- Reflexes are normal
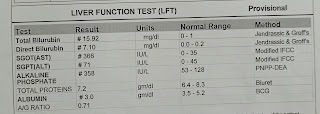
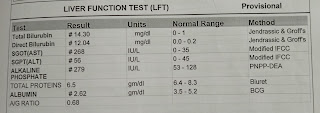
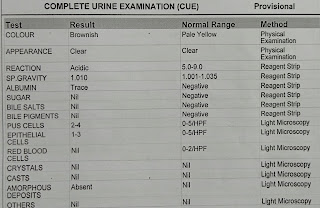
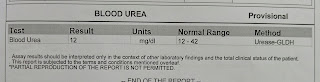
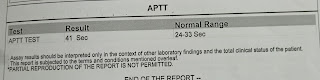
Investigations :
13/11/21
14/11/21
Diagnosis : Liver disease secondary to alcohol consumption

















Comments
Post a Comment